The Clinical Case for Nutrition
Science is increasingly showing just how critical nutrition is to healing and recovery. As we know during a state of trauma, such as injury or surgery, the body’s nutritional needs increase:
- The body enters a higher metabolic state and requires more energy 1
- Trauma and lack of use leads to muscle atrophy, which prolongs recovery 2
- The immune system is weakened due to stress and shock 3
- Risk of wound infection is increased 3
- Persistent inflammation delays return of function 4
- Trauma and physiological stress lead to increased fatigue 5
Nutritional deficiencies impede the natural progression of healing, including elevating the risk of infection and lengthening recovery periods. A patient that is nutritionally optimized will heal better and faster and have better long-term outcomes. One that isn’t will heal more poorly and more slowly and may have long-term complications.
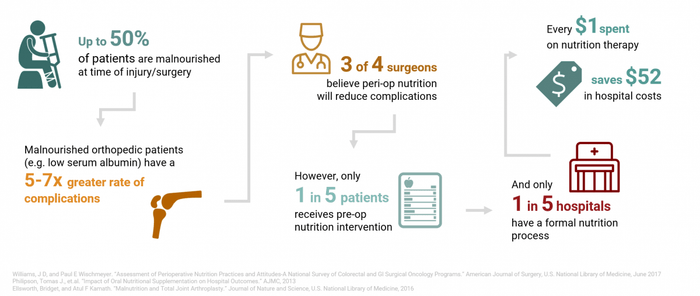
Unfortunately, most Americans are overfed and undernourished, meaning most Americans are not at optimal nutritional status to prevent complications post-trauma. Hospital studies have shown that as many as 50% of patients are undernourished or malnourished. These patients face greater complications than properly nourished patients, including longer hospital stays, greater risk of infection, and increased mortality.6 One study, published in the Journal of Nutrition, studied over 16,000 individuals and found that many are not meeting the minimum recommended thresholds for micronutrient intake (see below): 7
| Nutrient | % of Americans Deficient | Nutrient | % of Americans Deficient |
| Vitamin D | 93% | Calcium | 49% |
| Vitamin E | 91% | Vitamin A | 45% |
| Magnesium | 55% | Vitamin C | 37% |
Source: Fulgoni et al. (2011)
The combination of increased baseline nutritional needs post-trauma, from injury or surgery, and prevalent undernourishment means that most Americans are not well equipped nutritionally to heal.
The Impact of Malnourishment on Healing

Physical therapists have an important role to play in helping patients optimize their nutrition status to improve healing.
APTA Guidance on Nutrition
“Nutrition is part of the professional scope of practice for physical therapists”-APTA
The APTA acknowledges that diet and nutrition are core elements of the conditions that physical therapists manage. APTA’s position is that:
“… it is the role of the physical therapist to screen for and provide information on diet and nutritional issues to patients, clients, and the community within the scope of physical therapist practice.” (House of Delegates P06-15-22-17).
Many physical therapists are unaware that providing nutrition guidance is within their scope of practice, but it should be considering that APTA endorses it and it is in the best interest of the patient. Furthermore, in states such as New York, California and Michigan, PTs are exempt from any licensure requirements when recommending supplements, nutrition products and providing nutritional consult may even be a reimbursable expense.
State by State Guidance
The Center for Nutrition Advocacy maintains a database of state by state licensure requirements and exemptions as it relates to providing nutritional advice. Below is a helpful map of the current regularly landscape. PTs can use the website to look into specific laws and exemptions in their state: Center for Nutrition Advocacy

Legend
This map generalizes complex state laws and does not replace reading state laws.
| Red: | It is illegal to perform individualized nutrition counseling unless licensed or exempt. Effectively only RDs are eligible for licensure. |
| Orange: | It is illegal to perform individualized nutrition counseling unless licensed or exempt. There is a non-RD pathway for licensure. Check for exemptions. |
| Yellow: | It is legal for all to perform individualized nutrition counseling. Effectively, only RDs are eligible for state recognition. |
| Green: | It is legal for all to perform individualized nutrition counseling; there may be restrictions on medical nutrition therapy (a number of exemptions may apply e.g. recommending nutraceuticals is permissible in NY).. |
Disclaimer: Neither this map nor the information on individual state pages constitutes legal or career advice. This is a preliminary interpretation of language of state statutes and regulations, and cannot substitute for legal counsel.
Future Payment for Services Will Depend on Health Outcomes
In addition to the clinical and professional drivers for integrating nutrition into practice, as healthcare changes to a value-based care system, there are even greater economic and reputational drivers to integrating nutrition into practice.
The model of payment for health services is transforming. In recent years, Medicare and commercial payers have shifted from a traditional fee-for-service model to a value-based model. In the value-based model, payment is more closely related to patients’ health outcomes and the cost of care provided. As this trend continues, PTs will be more deeply involved receiving payments based on their performance and will need to articulate clearly their impact on patient outcomes.
Nutrition counseling can be a key differentiator that can improve your patients’ health outcomes and increase patient satisfaction, while reducing costs across the care continuum 8.

Source: APTA 9
More information can be found here: APTA: Value Based Care
Which Products to Recommend?
With hundreds if not thousands of supplement products on the market, how is a PT to know which products to recommend? We suggest paying attention to the following:
- Is there clinical evidence supporting the products?
- Are the nutrients in sufficient doses to be clinically efficacious?
- Are the products certified and produced to high standards of quality?
- Are other reputable medical practices using the products?
- Can the manufacturer provide references and/or testimonials?
MEND products meet these clinical and quality standards, and are being used by the leaders in orthopedics and physical therapy. To learn about how you can partner with MEND to improve patient outcomes and nutrition education, visit mend.me or contact the team at info@mend.me.
Sources:
[1]Şimşek, T., Şimşek, H. U., Cantürk, N. Z. (2014). Response to trauma and metabolic changes: posttraumatic metabolism. Ulusal cerrahi dergisi, 30(3), 153–159. doi:10.5152/UCD.2014.2653
[2]Appell, H. (1990). Muscular Atrophy Following Immobilisation. Sports Medicine, 10(1), 42-58. doi:10.2165/00007256-199010010-00005
[3]Kimura, F., Shimizu, H., Yoshidome, H., Ohtsuka, M., Miyazaki, M. (2010). Immunosuppression following surgical and traumatic injury. Surgery Today, 40(9), 793-808. doi:10.1007/s00595-010-4323-z
[4]Claes, L., Recknagel, S., Ignatius, A. (2012). Fracture healing under healthy and inflammatory conditions. Nature Reviews Rheumatology, 8(3), 133-143. doi:10.1038/nrrheum.2012.1
[5]Hall, G. M., Salmon, P. (2002). Physiological and Psychological Influences on Postoperative Fatigue. Anesthesia Analgesia, 95(5), 1446-1450. doi:10.1097/00000539-200211000-00064
[6]Barker, L. A., Gout, B. S., Crowe, T. C. (2011). Hospital malnutrition: prevalence, identification and impact on patients and the healthcare system. International journal of environmental research and public health, 8(2), 514–527. doi:10.3390/ijerph8020514
[7]Fulgoni, V. L., Keast, D. R., Bailey, R. L., Dwyer, J. (2011). Foods, Fortificants, and Supplements: Where Do Americans Get Their Nutrients? The Journal of Nutrition, 141(10), 1847-1854. doi:10.3945/jn.111.142257
[8]Allard, J. P., Keller, H., Jeejeebhoy, K. N., Laporte, M., Duerksen, D. R., Gramlich, L., . . . Lou, W. (2016). Decline in nutritional status is associated with prolonged length of stay in hospitalized patients admitted for 7 days or more: A prospective cohort study. Clinical Nutrition, 35(1), 144-152. doi:10.1016/j.clnu.2015.01.009
[9]https://www.apta.org/uploadedFiles/APTAorg/Payment/Reform/EvolvingPaymentSystem.pdf