What you need to know, and how you can prevent it
Joint Replacements are one of the most common surgeries performed. There are roughly 7 million people living with a joint replacement in the United States today, and as the population grows older and new technologies make the procedures safer and more effective, these numbers are rising fast. There are now roughly 1 million joint replacement procedures performed each year, a number expected to increase significantly in the coming decade.
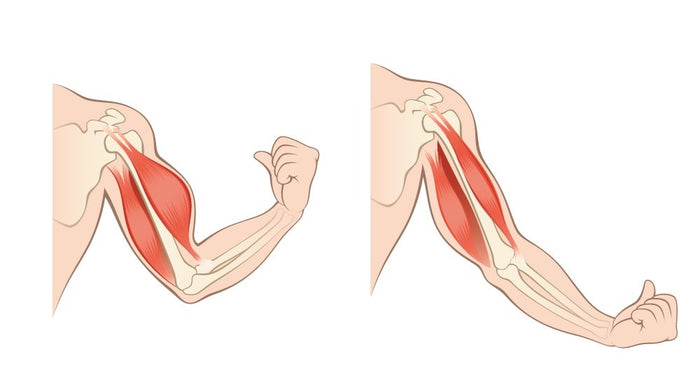
As with other orthopedic populations such as trauma, ACL reconstruction or rotator cuff repair, joint replacements can result in significant muscle atrophy and weakness (MAW) due to surgical shock and disuse. MAW can persist for years and delay return of function. Researchers are still looking to better understand the underlying muscle physiology mechanisms and the factors that lead to some patients experiencing MAW to a greater degree than others.
Prevention of MAW remains an important priority not only because of its impact on patient recovery and quality of life, but also because of the complications and associated costs to the healthcare system.
According to very large retrospective studies of more than100,000patients, MAW is quite prevalent and can persist for years, causing more than $8k in excess costs to the healthcare system on average for patients with muscle weakness. These costs are due to longer hospital stays, slower recovery, and increased rates of complications and readmissions. Orthopedic surgeons have attempted various techniques – such as electrical stimulation – to prevent muscle atrophy, however these techniques have shown little success to date.
A New Solution
MEND, a life sciences company based in New York City, has been working with leading hospitals to develop a new solution –MEND Joint Replacement– to combat muscle atrophy and weakness –a perioperative nutritional intervention (taken two weeks pre surgery and six weeks post) designed to promote muscle protein synthesis during the operative and immediate postoperative period.

Anumber of published placebo-controlled randomized trialshave shown that this approach reduces muscle atrophy, preserves muscle strength and improves return to function – with results showing as much as a66% reduction in muscle atrophyusing MEND vs. placebo –and more importantly,a faster return to function.
We are now studying the underlying mechanisms to better understand what is happening at the cellular level. A recent paper published in Applied Physiology by our research partners atSlocum Foundation, showed that there was a proliferation of muscle t-cells on the day of surgery. In other words, within 7 days of taking the product, there was an improvement in skeletal muscle. Furthermore, the research revealed a reduction in M1 macrophages post surgery, creating a more favorable inflammatory environment, placebo did not. This appears to be good news all around; better muscle, better function and reduced inflammation.
In Conclusion
There remains more work to be done to further understand the mechanisms and to understand if the solution will have a similar impact on other orthopedic populations. It is an exciting innovation that is safe, effective and low cost and that has important implications for outcomes in orthopedics. We are now advancing additional studies with leading hospitals and MDs to further develop the science on this solution.
References
[1] Wu et al.Demographics and clinical and economic characteristics of patients receiving total hip arthoplasy with and without muscle atrophy/weakness.ClinicoEconomics Outcomes Research, 2013.
[2] Chen et al.Association between muscle atrophy/weakness and health care costs and utilization among patients receiving total knee replacement surgery: A retrospective cohort study. Journal of Pain Research, 2013.
[3] https://mendjointreplacement.com/clinical-research/
[4] Dreyer et al.Essential amino acid supplementation in patients following total knee arthroplasty.Journal of Clinical Investivation, 2013.
[5] Muyskens et al.Cellular and morphological changes with EAA supplementation before and after total knee arthroplasty. Journal of Applied Physiology, 2019.